Your Support System
Pain, fatigue, and bone fragility are common symptoms of OI. These symptoms can lead to difficulties with participating in school and sports, and enjoying time with your friends. Learn about pain, fatigue, and bone fragility, how to manage symptoms and how these symptoms can cause stress.
In this module, you will read and see more about:
Your Support System
I. Having a Support System
Developing a support network
Different people can help you in different ways. You may find it easy to talk to your parents about the physical part of your condition. On the other hand, you might find it easier to talk to your friends, or maybe a future partner, about how it feels to have a chronic condition. You may also want a group of friends where you do not talk about your condition but share other interests. Developing a wide support system of people who you can count on when you need them is the best way to ensure all your needs are met. These people can include your family, partner, health care professionals, teachers, peers, and friends.
Trudy Wong, social worker, wrote a passage about the importance of having a support system, as shown in the Dream Machine book. The Dream Machine Is a novel written by Candace Amarante that tells the story of Skyler and her sister Ashling who has OI. Ashling helps Skyler cope with a fracture from a ski accident.

The following is an excerpt by social worker Trudy Wong from the novel, The Dream Machine explaining the importance of having a support system:
When we meet children with a chronic condition such as those with osteogenesis imperfecta (OI), we always try to meet their parents and siblings (when possible) as well. This is because we see our patients as part of several larger systems, the main one being the system of their family. Social workers look at individuals as a whole so will ask many questions. We strive to work with the children to make sure that they are doing well within the family, their groups of friends, or at school. We want to make sure that each person in the system is doing as well as they can be.
In this story (referring to The Dream Machine), Ashling and Skylar have the support and love of their parents but also of each other. By having gone through multiple fractures and surgeries with Ashling, Skylar and her parents had an idea of what to expect but this does not take away from the stress, anxiety and fear associated with every fracture. It shows us that the child with OI, family members and, in particular, parents are often the main care experts in their own situation. As health care workers, we need to be partners in care with families who have the experiential expertise of living with OI on a day-to-day basis.

The bond between the two sisters also shows us how important it is to have peer-to-peer support for patients. That is why both Ashling and her parents knew that she was the best person to tell Skylar that she would not be able to ski for a few months. There is something special about being reassured and comforted by someone who has gone through similar experiences. Social workers will always try to set this up for our patients if it can be helpful.
Finally, what was clear in Ashling and in Skylar, was the power and strength that comes from positive thinking and mindfulness. By using her imagination, Ashling has helped herself in painful situations over the years and in this story, she was able to use this gift and strength to help her sister as well. By seeing the way in which she helped Skylar, we see that Ashling is empathetic, resilient and determined, someone to be admired and a wonderful role model.
II. Talking to your Support System

Talking to your family or partner about OI
 When you feel better, you will be able to resume your daily activities and start taking more control of your condition. Your family or partner want you to be safe. However, you might feel that they are too protective of you. It is important to have an open and honest conversation with them about finding a balance between their role as a supportive caregiver and your need to make your own decisions.
When you feel better, you will be able to resume your daily activities and start taking more control of your condition. Your family or partner want you to be safe. However, you might feel that they are too protective of you. It is important to have an open and honest conversation with them about finding a balance between their role as a supportive caregiver and your need to make your own decisions. Talking to health care professionals about OI
If your doctor works in a clinic, there will be a “team” of professionals, such as other doctors, nurses, physiotherapists, occupational therapists, dietitians, social workers, and psychologists who can help you. Your doctor is a great source of information about OI. However, other members of your health care team have their own areas of expertise and can answer your questions about specific topics too.
If you think you might forget some of the questions, write them down before the appointment. For others, writing down the questions helps relieve some of their feelings nervousness. If your medical appointment may be an anxiety-provoking, check out the 🔗 Mental Health module for some helpful tips.
You might think your doctor is too busy or that your question is not really that important. Sometimes, you may feel more comfortable talking to another member of your health care team, like your nurse or therapist. Remember that your doctor or other health care providers want to make sure they answer all your questions about managing your health with OI. Having all your questions answered will ensure you make informed decisions about your health plan.
- Speaking alone with your doctor
Here are some video clips to help you understand better how to communicate with your doctor.
Watch this first clip of Brandon talking to his doctor.
The Doctor’s Appointment: Season 1, Part 1.
✓ How do you think this visit went?
Now, let’s look at a video of Brandon’s follow-up appointment with his doctor. As you watch the video, see if you can find three tactics that you could try for yourself.
The Doctor’s Appointment: Season 1, Part 2.
✓ How do you think this visit went? How is it different than the one before?
If you found yourself in this situation, would you feel comfortable addressing these concerns with your doctor on your own?
It is always a good idea to sit down with your parents ahead of your clinic visits to talk about the importance of speaking to your doctor on your own. That way, if you find yourself in a difficult or uncomfortable situation (similar to Brandon’s first appointment), you will feel more comfortable talking to your doctor.
The next two video clips should help you better understand how to assert yourself when speaking with your doctor.
Watch this first clip of Kaitlyn talking to her doctor:
The Doctor’s Appointment: Season 2, Part 1.
✓ How do you think this visit went?
Now, let’s look at video of Kaitlyn’s follow-up appointment with her doctor. As you watch the video, see if you can find three tactics that you could try for yourself.
The Doctor’s Appointment: Season 2, Part 2.
✓ How do you think this visit went? How is it different from the one before?
If you found yourself in this situation, would you feel comfortable being this honest and assertive with your doctor? Remember, deciding what you want to tell or ask your doctor ahead of your clinic visit will help you feel more prepared if you find yourself in a difficult or uncomfortable situation (similar to Kaitlyn’s first appointment)
- Tips for Talking With Your Doctor
Your doctors, nurses, and social workers have a really good idea of what will help with your transition to the adult health care system. Talking to these people can help prepare you for this change. Sometimes, it can be hard to talk with them, especially if your parents always did the talking!!
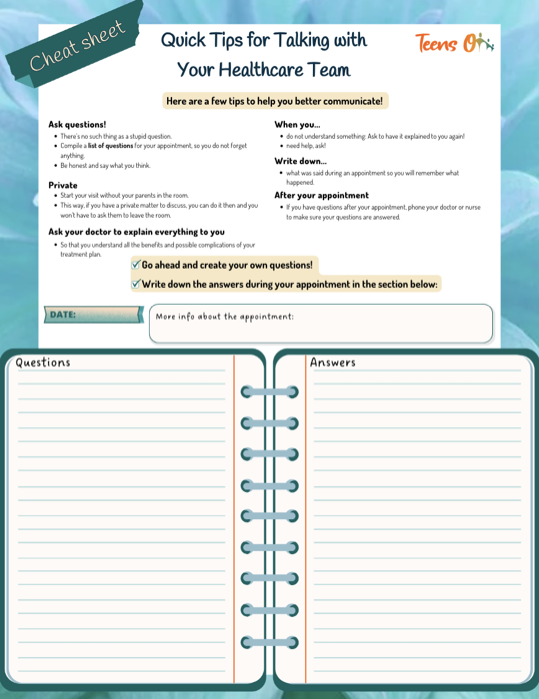
- Here are a few tips to help you better communicate with your doctor and health care team:




- Ask questions! There’s no such thing as a stupid question. Compile a list of questions for your appointment, so you do not forget anything.
- When you do not understand something, ask to have it explained to you again.
- When you need help, ask!
- Be honest and say what you think.
- Write down what was said during an appointment so you will remember what happened.
- If you have questions after your appointment, phone your doctor or nurse to make sure your questions are answered.
- Start your visit without your parents in the room. This way, if you have a private matter to discuss, you can do it then and you won’t have to ask them to leave the room.
- Ask your doctor to explain everything to you so that you understand all the benefits and possible complications of your treatment plan.
- 🔗 Download our guide to help you plan what to discuss at your next doctor’s visit!
Talking to teachers and school about your OI
It is important to communicate with your school. Let them know you have OI, how you manage it, and the adaptations you may need. This can be done alone or with the help of your parents/legal guardians or health care team, through meetings with your principal and teachers, by written notes, or by email. You can also involve your family members to help you navigate the conversation.
Your principal and teachers need to know that you have OI to make sure you can go to school, participate in activities, and realize your full potential in a safe way.
Later in this module you will find tools to help you 🔗 ask for help at school.
5 Tips to Talk About Your Health Needs at School!
Talking your peers about your OI
OI is a rare condition, so it may be hard to find someone who lives close by but does mean you would necessarily connect. A good way to connect with people that share the same life experience as you is by joining a chat group or online community. For example, you can exchange with people having OI. Some individuals said that it has helped them talking to someone who has been through what they have been through. They feel understood when the person is knowledgeable about OI. Keep in mind, though, that every person’s experience is unique and even if you are in touch with someone who has OI, it does not mean that everything they have tried or experienced is necessarily the best option for you. Importantly, always be careful when you share personal information online and when you set a meeting with someone you have only met online. To start, you can start with some of the online communities available by COIS, OIF, OIFE.
Talking with friends about your OI
Friendships are meaningful relationships that can improve your health and well-being. Friends provide you with social support through good and bad times, celebrate your successes, and help you overcome challenges. In addition to bringing you happiness as well as a sense of belonging and purpose, friends can also boost your self-confidence and self-worth.
You do not need many friends to have all these benefits. Always prioritize quality over quantity. A few truly close friends are enough. Remember that any friendship needs mutual effort. Treat others like you would like to be treated. Sometimes you are the one who needs support from your friends, while other times you are the one providing support. It is important to show to your friends your appreciation and how much you care about them.
However, we recognize that it is not always an easy task to maintain friendships. Sometimes, growing up makes it hard to nurture friendships and even more to develop new ones. Other commitments, such as college, work or family, can come into your way. You might also grow apart from your friends as a result of changes in your lives and interests. Some people with OI feel that their physical limitations prevent them from socializing as much as they would like to. The Internet can be a great way of keeping up with friends when meeting up in person is more difficult. If you are looking to make new friends, we encourage you to extend your social settings. For example, you can start volunteering or take up new classes, such as cooking, dancing or art classes.
III. Getting Help from your Support System
Different situations may arise when you will need help from your support system. Learn how to advocate for yourself, access your supports, use tools too communicate your needs, and deal with bullies.
Advocating for yourself
Do you often say yes when you mean no? Do you hold back your opinion or not stand up for yourself because you are afraid of confrontation or making waves?
Assertiveness means expressing your wishes, opinions, and feelings in a clear way while respecting the rights of others. It is not the same as aggressiveness, which does not respect the rights of others. It is also not the same as selfishness, which means only thinking about your own rights. Learning to be assertive will help you to gain self-confidence and the respect of others. You need to know that you are allowed to ask questions whenever you are unsure of something. Your doctors and nurses are there to help you, but they are not mind readers. If you have questions or if anything is bothering you about your treatment, talk to your doctor about exploring other treatment options. You are a person first, and not just a patient; what you want matters. Be assertive! Don’t be afraid to speak up for what matters most for you. Being assertive doesn’t always come easily and usually takes years of practice to perfect. Don’t get discouraged!
Dealing with bullying
Bullying is repeated, aggressive, and unwanted behaviour towards one person from another person or a group of other people. Bullying is hurtful and can occur in many different forms. Bullies can hurt someone physically, verbally, socially (through exclusion or spreading rumours), or electronically (for example, on social media or by text messaging). Some young people with OI have found themselves to be the target of bullies.
Here are some strategies and important points to keep in mind for coping with bullying.
- Ignore the bullying and walk away. Make them think you don’t care. This can also be very hard to do. If the bully knows they’re upsetting you, they’ll do it more, so use all your acting skills to pretend it doesn’t bother you.
- It’s crucial to recognize when you’re being bullied. Don’t brush it off or think it’s something you should just deal with on your own. Acknowledge that what’s happening to you is not okay.
- Talk to someone you trust, like your parents or legal guardians, a friend, a teacher, or a counselor. They can help support you and find ways to stop the bullying. If you talk to someone and they can’t help, then talk to someone else. Don’t give up! Bullying is a difficult problem and often it takes involvement of many people for it to stop.
- When you’re at school, try to stay in areas with adult supervision, like the cafeteria or the library. Being in these areas can provide you with a sense of safety and security, knowing that there are adults who can intervene if the bullying occurs.
- Remember, bullying doesn’t define who you are. Focus on your strengths and the things you’re good at. Building your self-esteem is key to weathering the storm. Take time for activities that uplift and affirm you, whether it’s indulging in hobbies, surrounding yourself with supportive friends and family, or practicing self-care. Prioritizing activities that boost your spirits can help sustain your emotional well-being during tough times like bullying.
- Take advantage of any anti-bullying programs or support groups offered at your school or elsewhere (e.g., online). Connecting with others who have similar experiences can be empowering.
- It’s okay to assert yourself in a non-aggressive way. Practice assertive communication and set boundaries with the bully. Let them know their behaviour is not acceptable.
- If you’re struggling to cope or the bullying is taking a toll on your mental health, don’t hesitate to seek help from a counselor or therapist. They can provide support and guidance to help you through this tough time.
If you feel comfortable, you can share your experiences and advocate for policies and procedures that promote a safe and inclusive school environment. Your voice matters.
Accessing supports
There are lots of supports available to help you deal with your OI at the hospital, in your school, and within your OI community. An important source of support is your OI team. The social worker, nurse coordinator, and occupational therapist can assist in finding resources for school, work, and financial issues related to medication costs, adaptive equipment, or orthotic devices. They can help you access these resources as well as many others. Your family or significant others and trusted friends are other good sources of support. There should also be support in your school, such as guidance counselors, social workers, and psychologists. The OI community also has a variety of resources available for supports in your local community.
Further reading:
The School of No Fun and No Play: Learning How to Create Supportive Environments from Children with Osteogenesis Imperfecta
Cleary, B., Linds, W., Carnevale, F. A., Thorstad, K., Rauch, F., & Tsimicalis, A. (2024). The School of No Fun and No Play: Learning How to Create Supportive Environments from Children with Osteogenesis Imperfecta. Journal of Disability Studies in Education (published online ahead of print 2024). https://doi.org/10.1163/25888803-bja10027
Asking for Help at School
Regular vs specialized schools
You may have been going to a specialized primary school and may now be considering going to a regular secondary or high school. Or, you may have always gone to a regular neighborhood school. Either way, studies have found that individuals with OI enrolled in regular schools progress academically at the same pace as their peers who go to specialized schools. In addition, they participate actively and excel in extracurriculars and school activities.
Resources to help you
- Having extra time to complete classroom assignments
- Completing tasks or presenting information in other ways (e.g., through taped answers, demonstrations, dramatizations, role play, taking exams orally)
- Recording your lessons so you can review them at a later time, having handouts of class notes, or getting photocopies of the teacher’s notes
- Getting a variety of learning tools such as special computers to make it easier for you to complete your assignments
- Having an extra set of books so you do not need to carry them to and from school
- Being able to have a scribe, which is someone who writes for you when you cannot
- Having access to the elevator if your school has several floors
- Leaving the class early to avoid crowded hallways

Like for the IEP, either your parents/legal guardians or your teacher can request that an OI Individualized School Plan be written for you with your input and that of relevant professionals and specialists. Here are some examples of accommodations that might make it easier for you at school:
- Having a fracture response plan
- Having a mobility plan (e.g. understanding how your mobility may change because of your pain, fatigue, fracture or weather)
- Identifying who may help with wheelchairs transfers
- Identifying who may help with toileting and clothing
- Having a physical education plan (e.g. for class, extracurricular activities, outdoor play)
- Having a transportation plan
- Creating a school evacuation plan
- Having preferential seating in the classroom